THE NUMBER of care and NHS staff who died as a result of workplace infection with Covid is probably around 3.5 times higher than Public Health Wales statistics state.
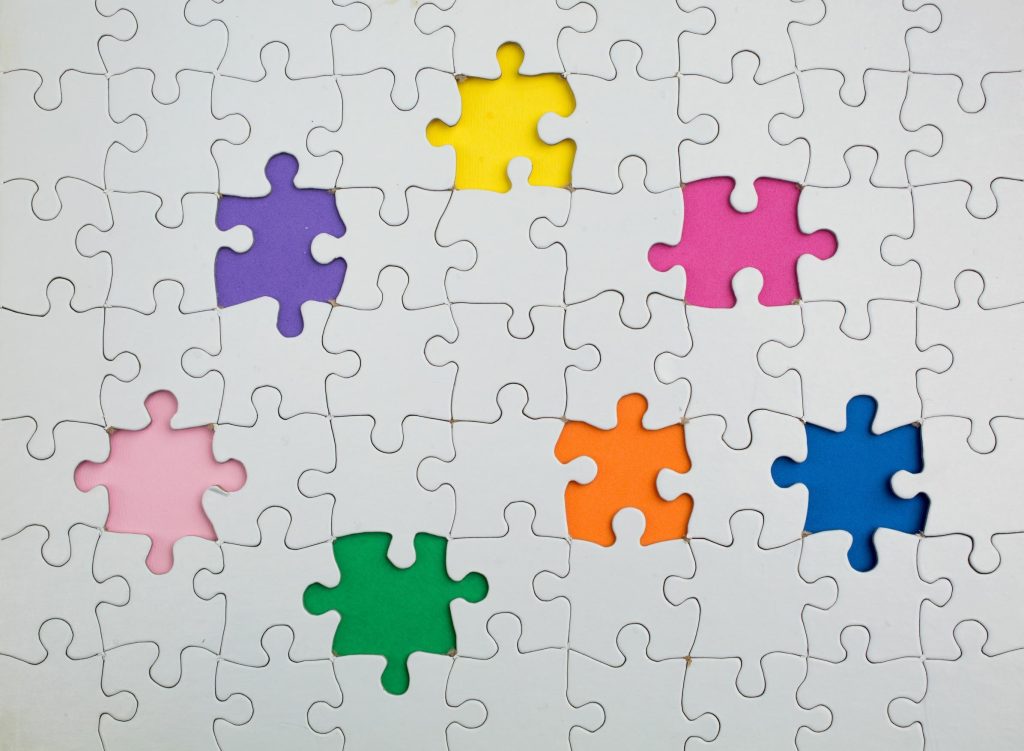
However, no definitive figure is available. A form used to capture vital data failed to capture the information needed, as important questions could be left incomplete. That means the statistical basis for the Welsh Government’s response to the pandemic was out of kilter with reality and led to poor-quality decisions.
FORM FILLING FAILURE
The reason for the understatement is as mundane as it is unbelievable.
In April 2020, Public Health Wales (PHW) rolled out a form to record detailed data about Covid fatalities. The form’s design allowed clinical staff to record key data about each death. Alongside basic data, such as age and sex, the form had a check box to indicate if the deceased was a key worker. However, the form was often only partly completed, and almost a fifth of the information it was intended to capture was missing from the final data.
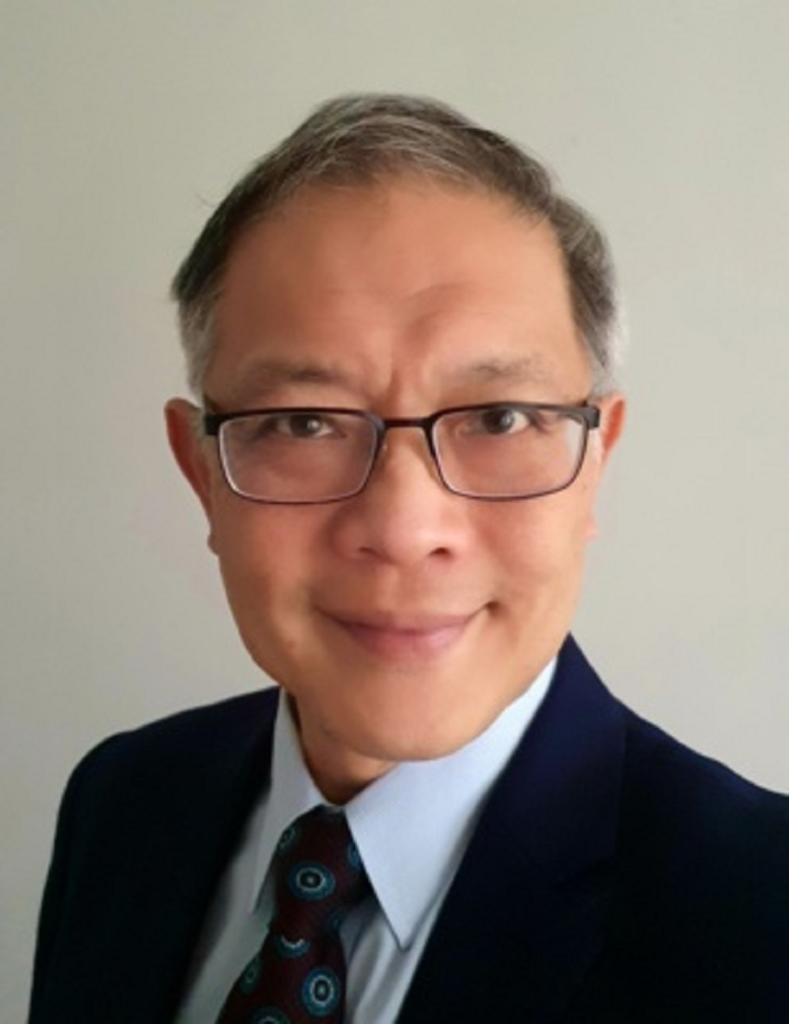
Professor Fu-Meng Khaw confirmed the position while giving evidence to the third module of the UK Covid Inquiry on Tuesday, November 5.
The professor is the National Director of Health Protection and Screening Services and Executive Medical Director for Public Health Wales. He joined Public Health Wales in March 2021. The Inquiry’s third module is considering the pandemic’s impact on healthcare systems.
At the pandemic’s outset, Public Health Wales was able to ascertain the number of people suffering from Covid in Wales. However, once the pandemic took hold and the number of infections increased, it encountered problems in handling data and obtaining the details needed to assess its progress among different groups.
The pandemic’s rapid spread and the need to gather data also encountered another problem: Welsh NHS bureaucracy. Vital data was routinely not available to the Welsh Government or NHS Wales until clinical coding took place three months post-event. In the pandemic’s context, that created a huge and potentially dangerous lag between a patient’s death and detailed information being received to inform pandemic responses.
THE INFORMATION DEFICIT
As things stood at the time, the Welsh Government, Public Health Wales and health boards realised that the information coming from clinical settings about the pandemic was incomplete and unreliable.
Baroness Hallett, the Inquiry Chair, pointed out that the information gap meant that Public Health Wales had virtually no idea of what was going on in the community. Professor Khaw agreed with her assessment.
To resolve those problems, throughout April 2020, Public Health Wales, the Welsh Government and health boards worked together to construct an electronic reporting form. The form captured crucial real-time data and would’ve been a valuable tool in tracking the impact on Welsh healthcare and whether particular groups were more at risk than others.
The form was rolled out on April 23, 2020. It was accompanied by supporting documents, instructions, and a training video on its use.
The form recorded 6,514 deaths throughout its life. However, over 1,000 elements of data are missing in the question about key worker status.
The form asked, “Was the patient a key worker?” Five different buttons were displayed, one of which was “a healthcare worker.”
Despite that, Professor Khaw told the Covid Inquiry: “We do not hold data in respect of the number of staff within healthcare settings in Wales recorded as having died of COVID-19.”
The data on the form records 36 deaths from Covid among health and social care staff during the pandemic. However, more reliable Office for National Statistics information, compiled from more solid clinical data, estimates there were at least three-and-a-half times that number.
WG IGNORED EXPERTS ON COVID IMPACT
The Welsh Government also significantly overestimated the “reasonable worst-case scenario” and its impact on the Welsh NHS’s ability to function. Despite Public Health Wales experts advocating for a 25% likelihood of the “reasonable worst-case scenario”, the Welsh Government chose a higher 40% probability of it. During the pandemic’s critical first phase, the Welsh NHS experienced only 7% of the worst-case scenario.
That means the Welsh Government over-engineered its response to the pandemic. What the Welsh Government planned for did not happen.
The wider consequences are the over-commitment of scarce resources in a public health emergency and the claimed impact of the pandemic on Welsh NHS capacity being less than the Welsh Government chose to predict and subsequently claimed.
It could be argued from the above that the pandemic’s impact on the Welsh NHS was less than expected and claimed. If that’s not the case, it suggests the Welsh NHS’s pre-pandemic condition was worse than the Welsh Government acknowledged at the time and afterwards, which led, in turn, to its continuing performance failures.
SYSTEMIC FAILURE
Despite Public Health Wales’s central role in responding to public health emergencies, it was omitted from discussions and decisions on key elements of the pandemic’s handling in Wales.
There were more than 10,000 probable or definite hospital-acquired cases of Covid in Wales over the pandemic period.
In December 2020, a senior public health official in Wales reported: “Organisations and bodies will pressure us to take more precautionary measures.
“The confidence of staff in high intensity units is being lost. If there is a high-risk pathway we should take precautionary measures.”
But nothing was done.

By that time, it was widely known that ventilation was an essential element to control Covid’s spread. However, Public Health Wales was not consulted on how it might be implemented. The division of responsibilities with Welsh NHS bodies, advisory groups, ad-hoc Welsh Government working groups, and Welsh NHS executives and ministers meant lines of responsibility were blurred and responsibility diluted.
As an example, Public Health Wales did not issue any guidance on restricting hospital visits by patients’ relatives. Instead, a hospital visiting group established by Wales’s Chief Nursing Officer advised the Welsh Government on the issue.
While absence of evidence is not evidence of absence, Professor Khaw had no evidence that the important role of a patient’s family was ever taken into account when deciding to restrict visiting.
Neither did Public Health Wales provide advice about any aspect of the support or health advice that should be offered to those who were shielding or their families.
It didn’t because it was never asked.
If the body supposedly responsible for Wales’s public health, and incidentally for the Welsh response to disease outbreaks, was not asked for its advice, who was?
The picture of health administration in Wales that has emerged from the Covid Inquiry is one of an NHS over-loaded with bureaucracy, blurred or non-existent lines of responsibility, administrative waste and duplication, an inability to ensure essential information is recorded, and data practices that mean ministers may as well stick a wet finger in the wind to determine its reliability.
The need for a Wales-specific Covid Inquiry has never been clearer. The more layers are peeled away to expose the workings underneath, the more obvious the urgency of top-to-bottom Welsh NHS reform is.